In the race to 3D print and transplant seemingly every part of the human body, the esophagus has been a particular challenge for scientists and doctors.
But a team of Japanese researchers has now successfully transplanted a bio 3D Printed esophagus into rats.
The esophagus, which was printed using Cyfuse’s bio 3D printing software Regenova, maintained its structure after the transplant and even grew to be covered by natural tissue.
These findings by the Nagasaki University-based group could mean big strides toward the first 3D-printed esophageal transplant (esophagectomy) in humans.
Why Esophageal Transplants Are So Complicated
An esophagectomy is the main treatment for esophagus cancer. The operation involves removing all or part of the esophagus, then restructuring it using part of another organ (like the stomach or colon).
However, this method can lead to complications including acid reflux, abnormal narrowing of the esophagus, and dumping syndrome (when food moves too quickly from your stomach to the small intestine).
The materials used in these operations typically have low biocompatibility and are done via decellularization. This is when the intracellular parts of tissue are removed so all that remains is the exterior “skeleton” which can then be used in tissue regeneration and the creation of artificial organs.
While there is nothing wrong with this method and it’s been used in several successful esophageal-related studies, it does require using existing tissue. The benefit of the 3D printing technique is that the esophageal structure can be constructed using only cells.
New Technology For New Tubes
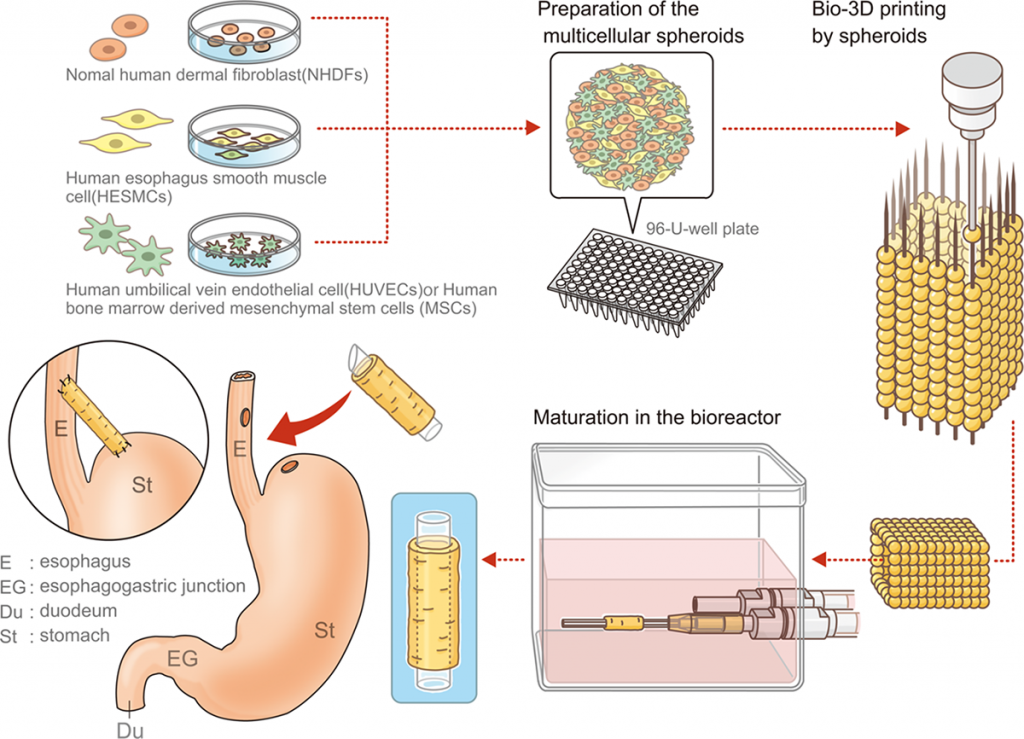
The Japanese team opted instead to print and install a scaffold-free and more tubular structure into their rats. The tube was made with a Regenova bio 3D printer using the Kenzan method. This process first assembles human cellular spheroids into the desired 3D shape. Then, the shape cultures in a bioreactor until the spheroids fuse together to achieve the appropriate strength and structure.
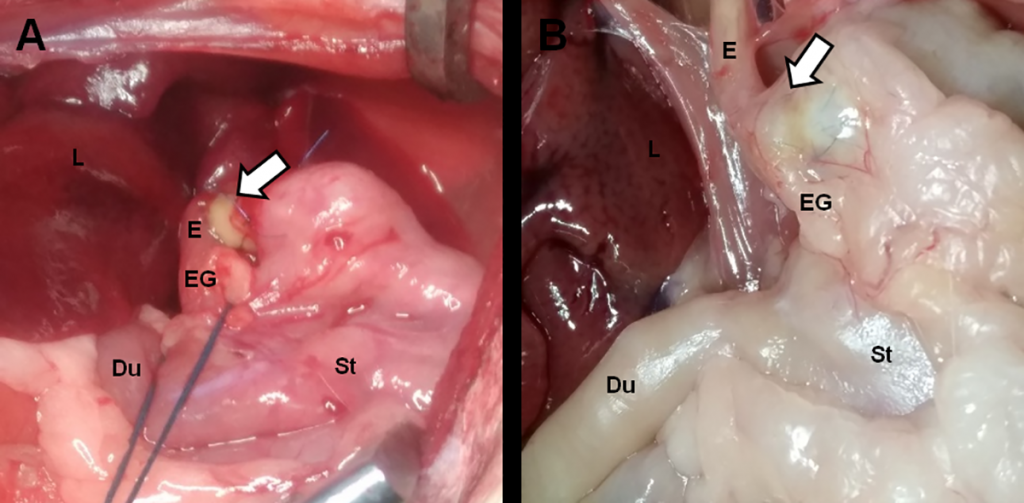
After testing for strength and flexibility, they were then transplanted into five male adult rats. Each rat survived and their esophagi maintained their shape and structure with no signs of leakage or perforation even after being exposed to gastric juices after eating. More remarkably, after 30 days scientists couldn’t detect where the rats’ natural esophageal lining and the transplanted structure began, as it became completely engrafted with natural cells.
What’s Next?
Researchers cautioned in their conclusion that despite the encouraging results, their esophagi did not perform as well as natural ones. However, the possible benefits of these results extend far beyond your food tube.
While it’s still early, using 3D printed biological and scaffold-free structures could decrease the amount of complications that come with more traditional transplant methods. No longer would patients have to sacrifice part of one of their organs (or someone else’s) to have a healthier esophagus. In times of organ shortages, this technology would obviously be vital in saving lives.
The researchers stated in their conclusion that the next step will be longer post-transplant assessment periods as well as orthotopic esophagus transplantation into larger animals.
Discuss this and other 3D printing topics at 3DPrintBoard.com or share your thoughts below.
Sources: Mayo Clinic | PLOS ONE