In Australia, vascular surgeon, Jason Chuen understands that 3D printing is the exciting next step in personalized medicine, which is why he uses 3D scans and 3D printing to deliver anatomical models. During an interview with 3DPrint.com, Chuen, who is also the Director of Vascular Surgery at Austin Health and Austin Health’s 3D Medical Printing Laboratory (3D Med Lab), suggested that “there is a lot of interest because the field of 3D printing in medicine is growing; we are seeing the doctors and researchers involved more than ever, as well as more application development originating from clinicians.”
In Australia, vascular surgeon, Jason Chuen understands that 3D printing is the exciting next step in personalized medicine, which is why he uses 3D scans and 3D printing to deliver anatomical models. During an interview with 3DPrint.com, Chuen, who is also the Director of Vascular Surgery at Austin Health and Austin Health’s 3D Medical Printing Laboratory (3D Med Lab), suggested that “there is a lot of interest because the field of 3D printing in medicine is growing; we are seeing the doctors and researchers involved more than ever, as well as more application development originating from clinicians.”
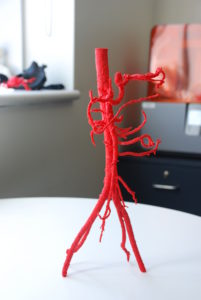
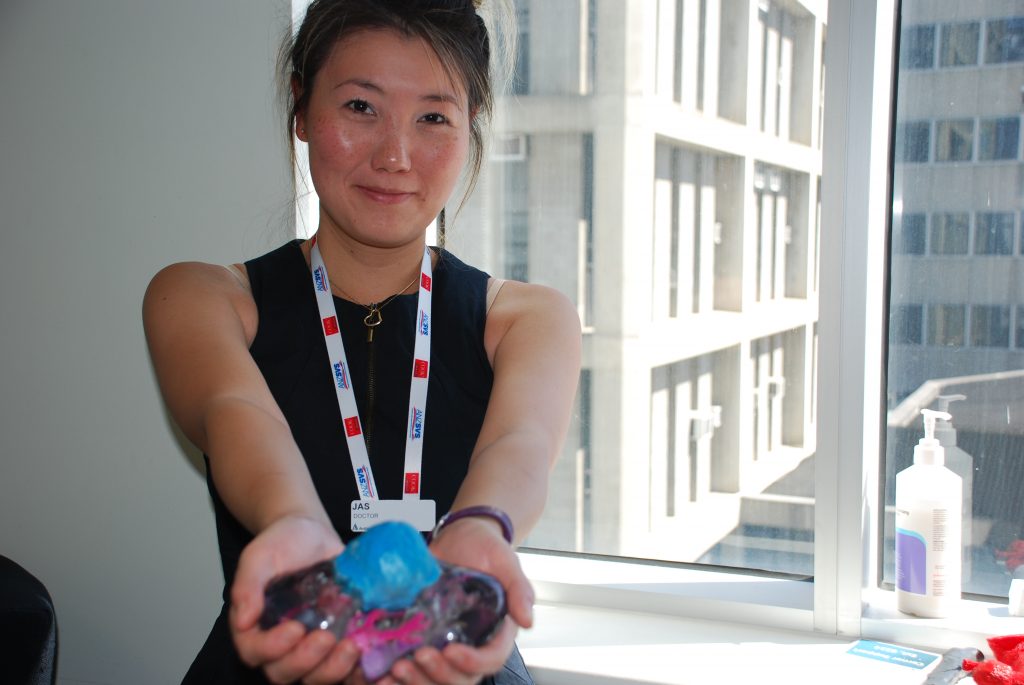
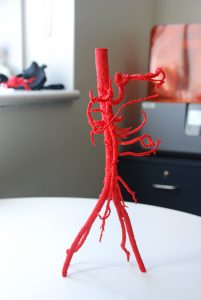
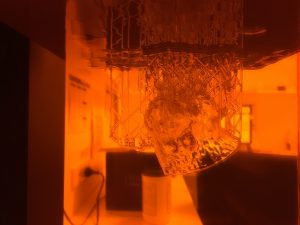
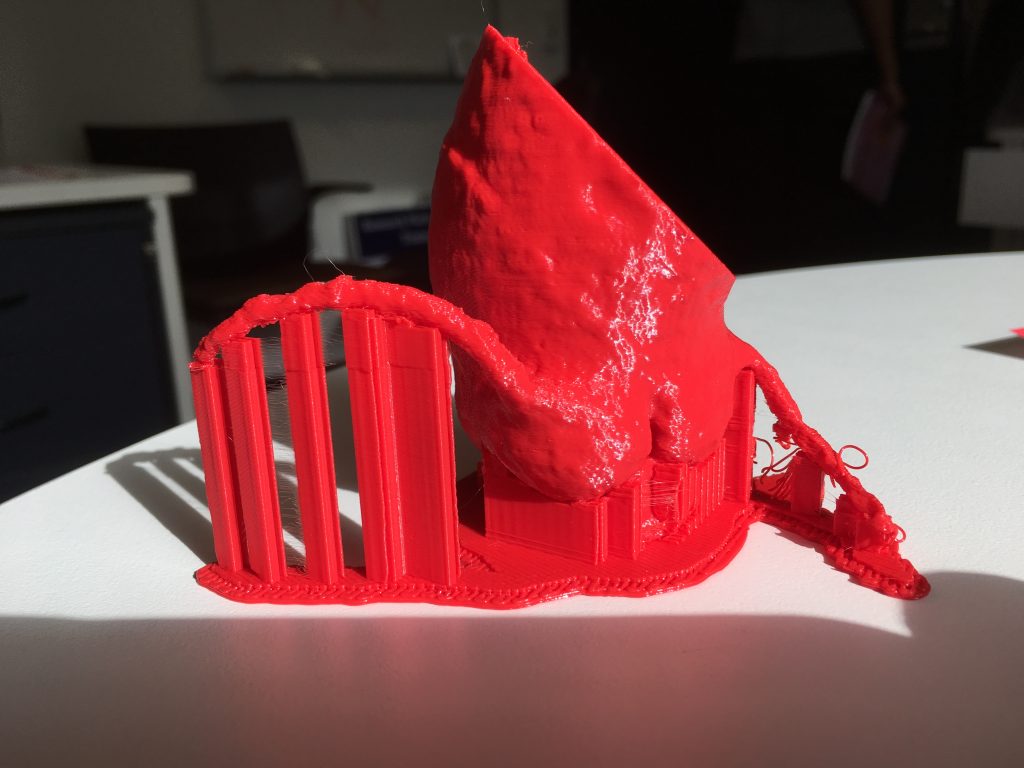
At The University of Melbourne, in Australia, the 3D Med Lab supports 3D printing for clinical applications and runs an active research program exploring how it can be used for teaching, procedural simulation, patient education, surgical planning, and prosthetic implants. The first facility of its kind in Australia, 3D Med Lab, frequently prints models of diseased aortas to perform a “practice-run” of surgery. What makes this lab unique is that it is hospital-based, and works with many different specialties. Chuen has been looking into the landscape of medical 3D printing for many years and earlier this month along with his colleague Jasamine Coles-Black, a Doctor and Vascular Researcher at the Department of Vascular Surgery at Austin Health and the 3D Med Lab, organized the fifth annual 3D Med Australia Conference, which he claims is the only meeting of its kind in Australasia, with only one or two more around the world of a similar nature, like Materialise‘s medical 3D printing meetup in Belgium.
Chuen and Coles-Black even begun printing out copies of patient kidneys to help surgeons at Austin Health plan the removal of kidney tumors. Moreover, Chuen understands that the immediate challenge in medical 3D printing is ensuring that medical professionals themselves are up to speed with the technology because it is their clinical experience that will drive new applications and projects.
During our interview, Chuen asserted that the conference has once again proved that Australia is leading the way with cross institution development cooperations, ethical issues surrounding 3D printing and he looks forward to many exciting possibilities of the technology for the future.
Why was the 3D Med Conference so important to the region?
We noticed there were a lot of groups that existed previously that didn’t know about each other and the meeting has become a really good focal point for people to find out about what others are researching and selling. So rather than working on their own and almost in secret, they can join together and create projects that cross different institutions, specialties and disciplines. During the conference, at every corner I encountered groups of people from different universities and cities gathering to hatch a project, proving that there was a very cooperative atmosphere. They all clearly had common interests and discovered that they can work outside of their own space with others.
What was so unique about the 3D Med Conference?
Because there really aren’t many meetings like this, the areas of interest are still growing, anyone who is working with these technologies have applications in different areas so that is why we have a lot of crossover between the fields. The strength of the confreence comes from encouraging people to have an overview of what was happening in the field, so rather than just understanding technical aspects of technology, everyone started to become knowledgeable about the whole landscape, for example, why we need to care about ethics and regulation, or considering the useful implications of applying techniques from a different area of science and research.
One of the biggest challenges for 3D printing is?
One of the big problems in customized medical devices and the 3D printing space is that there is uncertainty about what will happen in the future. Apart from the guidance of the US Food and Drug Administration (FDA), there hasn’t been a lot of resources for manufacturers and researchers on how 3D printing and customized medical devices will be regulated. Australia’s own Therapeutic Goods Administration (TGA) representation in the International Medical Device Regulators Forum (IMDRF) has been very strong,particularly around 3D printing and customized medical devices. During the conference John Skerritt, Deputy Secretary of the Australian Department of Health, outlined the broad framework around the field and has engaged in a consultation process with the medical 3D printing community (and we have provided some proposals for the final documentation that will be ready soon.)
Distributed production will present new risks for ensuring the quality control of end products. It will need a fundamental shift in responsibility from the supplier to wherever the medicines or devices are manufactured. That represents a huge change and we have to work out how it could work. But if we get the regulation right then it will transform access to medical products.
What does the future of 3D printing in medicine look like?
The whole point of what we do is improve patient care, so we have to think very carefully about our next steps and analyze whether it is helpful or not. For patients, anatomical models help them see and understand the condition or surgery they plan for. We have done projects and have some conclusive evidence that patient understanding is improved with anatomical 3D printed models.
Patients are interested to know what will happen in the future, especially with 3D printed kidneys and stents. But the truth is that that technology is very far away. We may never be able to 3D print an organ, not at least the way we imagine it to be. Realistically, if we are talking about an organ for transplantation, we have to think that no matter what the organ looks like, the question is: does it do the job? For example, if we were thinking about bioprinting in order to replace a kidney, as long as it performs the function of the kidney, it doesn’t matter what shape it comes in. And for that, we have to be able to reproduce a structure. This could be in shapes, rather than in one block, or it could be a composition of an external and an internal device, meaning we would be looking into something that is assembled. Today the technology to have the replacement kidney is available, it is a dialysis machine, yet you wouldn’t expect a dialysis machine to look like a kidney. The same is going to happen with 3D printed organs, where we need to separate the appearance and structure of the organ from the function. In the end, the function is what matters.
As such, if we were to imagine what a 3D printed heart would look like, we would need to go into the field of soft robotics or mimicking natural structures, all of that changes fundamentally how we think about organs for the human body.
How can your particular medical field benefit from 3D printing?
As a vascular surgeon, I’m also looking at 3D printed stents, and there is quite some work around that. Mainly it is based on printing something that looks like a stent, but it is very difficult to reproduce the mechanical properties of a stent using 3D printing. The benefits revolve around the different materials that could be used with 3D printing, for example, if you could reproduce a stent in a bioabsorbable plastic it would allow surgeons to deploy it with embedded drugs (like antibiotics and pain medication) that get released at a set time. There are a lot of options in terms of using multi material technology in customized implant production, as well as great precision, and that is an area where 3D printing helps.
Ideally, we need to understand the technology to know where the errors can happen. But in general, it is improving, both in hardware and software, the challenge will be about making it accessible. We have done randomized trials around anatomical models for teaching, education and simulation. There are already some 3D printed medical devices, such as for joints and implants. It would be ideal to have assessments of the economics to determine whether the anatomical models will be worthwhile.
How is Australia changing the paradigm of medical 3D printing?
Australia has world leading technology, but in terms of the way we have collaborated and worked together, we are quite unique. Even globally one of the big problems is finding the groups that are doing this kind of work. We have been in touch with research groups in Poland, Boston, and Toronto, even engaging with large centers like the Mayo Clinic, in Minnesota. Key collaboration between international centers are great and we are keeping an eye out for other major hubs of activity, like in China, South Korea, and Europe. We need to link up all the international groups, that’s where we see things are going!
[Image credit: 3dMedLab, Austin Health]
The post Interview with Jason Chuen: Shaping Australia’s Medical 3D Printing Environment appeared first on 3DPrint.com | The Voice of 3D Printing / Additive Manufacturing.